Professor of Rhinology & Skull Base Surgery, Ain Shams University, Cairo, Egypt
Department of Oto-Rhino-Laryngology, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
10- Endoscopic Surgery for Fungal Sinusitis
Fungal rhinosinusitis is an inflammatory disease of the mucosa of the nose and paranasal sinuses caused by different types of fungi. It is relatively uncommon but recently showing increasing incidence. It may occur in healthy patients. Aspergillus is the most common pathogen, but mucormycosis, histoplasmosis, and coccidiomycosis can occur. Immunosuppressed patients are at the highest risk for serious fungus infections, especially for mucormycosis.
Classification:
Fungal rhinosinusitis is classified into non-invasive and invasive types.
A. Non-invasive type: is extramucosal fungal infection (Fig. 1) and is classified into:
- Saprophytic: on dried secretion or blood crust.
- Fungus ball (mycetoma).
- Esinophilic Mucin Rhinosinusitis (EMRS).
- Allergic Fungal Rhinosinusitis (AFRS).
B. Invasive type: is intramucosal fungal infection(Fig. 2) and is classified into:
- Acute (fulminating) type.
- Chronic Invasive (indolent) type.
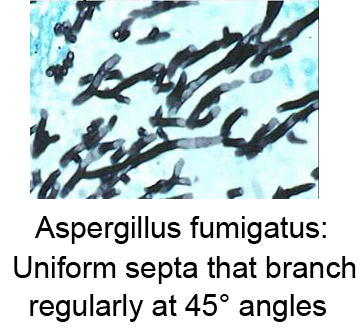
Aspergillus is a common saprophyte found in soil, dust, and decaying matter. Histological evaluation may show the characteristic uniform septa that branch regularly at 45? angles (Fig. 1). Aspergillus infection of the sinuses is usually extramucosal and noninvasive, but invasive fulminant forms do occur. The noninvasive type usually involves a single sinus, most often the maxillary sinus.
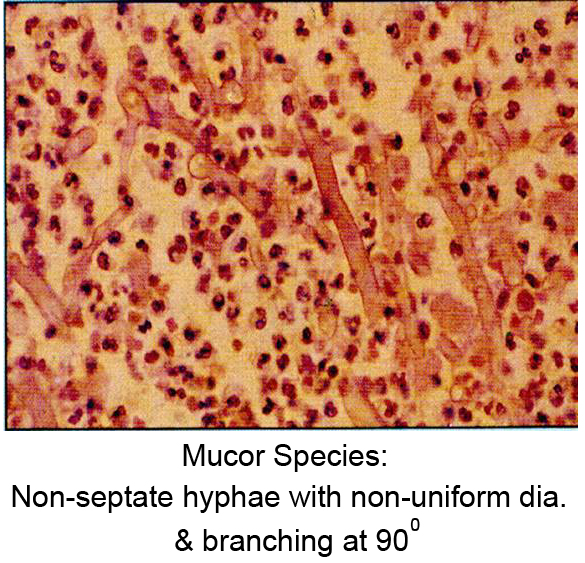
Mucor Species are non-septate hyphae with non-uniform diameter and are branching at 900 (Fig. 2).
Diagnosis:
Initial findings are unfortunately nonspecific, but subsequently, a characteristic viscid sometimes black nasal discharge may occur. Thick fungal debris and mucin (a secretion containing carbohydrate-rich glycoproteins) are developed in the sinus cavities. Polyps are common with EMFS and AFRS.
Radiograph evaluation of fungal disease is demonstrated best on CT. High-attenuation calcifications within the diseased sinus can be seen. A distinct fungus ball usually does not occur since chronic mucosal thickening surrounds the area of extramucosal fungal infection. Bone destruction occurs in the more invasive forms of fungal disease, and the appearance in immunosuppressed patients can be quite similar to malignant tumors.
MRI findings are related to inspissated secretions. A T1-weighted image through the opacified sinus shows mucosal thickening with isointense signal that increased with contrast and a non-enhancible hypointense lumen. Proton density and T2-weighted images demonstrate mucous along the lateral margin of the sinus and a low-signal-intensity region bridging the sinus cavity. Normal mucous and bacterial secretions have high signal intensity related to the high water concentration. The low-signal regions are related to the fungal infection and dehydrated inspissated mucous, calcifications, and iron salt deposition.PowerPoint Video= Diagnosis Of Fungal Sinusitis
Treatment:
Symptomatic fungal infections usually require
surgical intervention for complete cure; therefore, radiologic evaluation is
important. Aspiration of the sinus yields a thick greasy material, but cultures
rarely demonstrate the pathogen. Surgery, usually endoscopic, is often necessary
to remove all the infected material.
None-invasive fungal sinusitis is managed endoscopically with wide sinusotomy
and removal of mycetoma and in esinophilic type with polypectomy and aspiration
of all fungal mucin so that the inciting allergen is no longer present.
Recurrence is not uncommon once the disease is removed.
Invasive and fulminant fungal infections occur more commonly in immunosuppressed
patients. These infections are characterized by unrestricted spread of the
fungus beyond the sinuses into the orbits, cranial bones, neural foramina, blood
vessels, and brain. Cavernous sinus thrombosis or carotid occlusion can occur
due to infiltration of the skull base.
Mucormycosis is an uncommon sinus infection but is a much more severe fungal
infection that occurs in diabetic and immunosuppressed patients. There is direct
invasion of the mucosa with vascular involvement and thrombosis. Extension into
the brain can be quite rapid. Surgical intervention and antifungal therapy must
proceed quickly following the diagnosis. Correction of immune status is
mandatory in immunocompromised patients. Hyperbaric oxygen therapy can be of
value.
Chronic invasive fungal sinusitis is an indolent granulomatous lesion occurring
mostly in immunocompetent patients with progressive destruction of the bony
sinus walls resulting in orbital and/or intracranial extension of the disease.
Endoscopic surgical excision usually in multiple debridement sessions is the
main line of treatment. Orbital exenteration is usually needed but its timing is
usually difficult to determine as vision remains serviceable for many years.
PowerPoint Video= Treatment of fungal Sinusitis
Video1 demonstrates Endoscopic Sinus Surgery in a 42 y.o. female patient with right sphenoid fungal ball (mycetoma). The sinus mucosa around the ball was edematous while the rest of the sinus mucosa being rather normal.
Video1: Sphenoidotomy for Fungal Ball
Video2 demonstrates Endoscopic Sinus Surgery in a 11 y.o. patient with recurrent non-invasive Esinophilic Mucin Rhinosinusitis with polyposis. Sites where friable and severely diseased mucosa have been removed showed resistance for recurrent disease.
Video2: FESS for Esinophilic Mucin Rhinosinusitis with polyposis
Video3 demonstrates Endoscopic Sinus Surgery in an adult female patient suffering from Chronic Invasive Fungal Sinusitis. This patient underwent External Ethmoid Operation in 1998 which failed to cure here, then underwent 5 endoscopic debridement surgery till 2004 with no way to offer long-lasting control of the disease. The question of orbital exenteration has been always considered, however in presence of good vision, it has been regularly postponed.
Video3: Endoscopic Sinus Surgery for Chronic Invasive Fungal Sinusitis